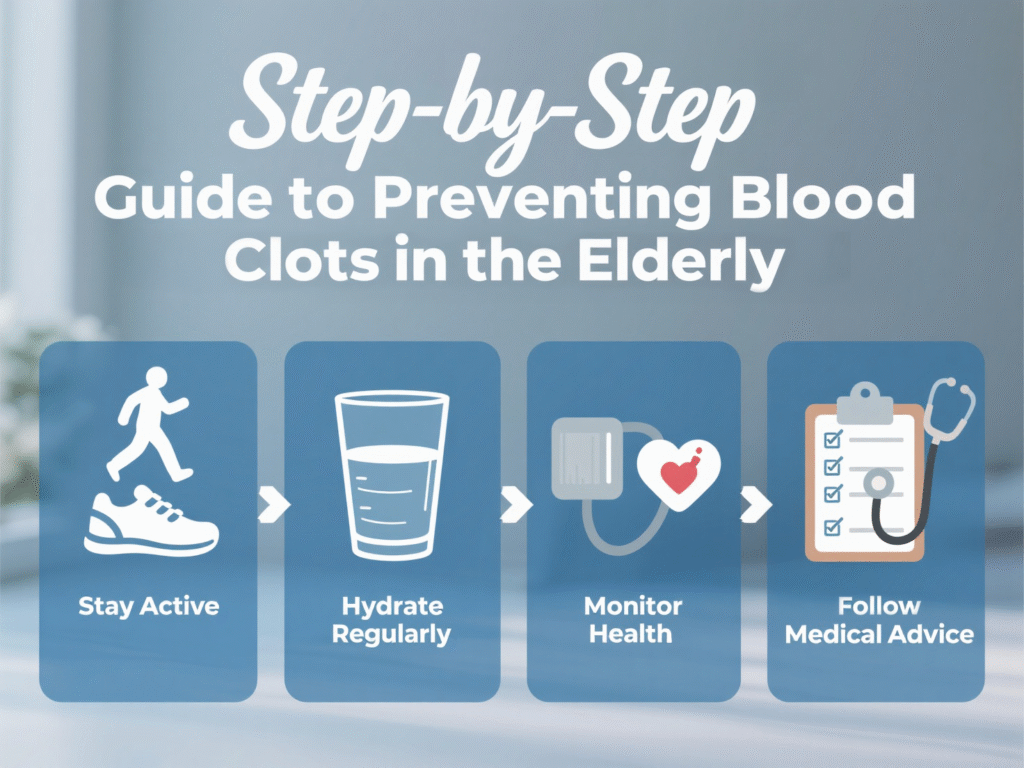
Step-by-Step Guide to Preventing Blood Clots in the Elderly
What Are Blood Clots and Why Are They Dangerous?
Blood clots are like the body’s emergency stop button for bleeding — and under the right circumstances, they save lives. But when they form unnecessarily or travel to critical organs, they can become deadly. Picture a clot as a traffic jam in your bloodstream. If it clogs an artery or vein, it can stop oxygen and nutrients from reaching your brain, lungs, or limbs.
The risk? Stroke, heart attack, pulmonary embolism — serious stuff that can change a life in minutes.
Why the Elderly Are at Higher Risk
As we age, our bodies change — and not always in ways we’d like. The elderly often:
- Move less
- Have slower blood circulation
- Take medications that affect clotting
- Undergo surgeries more often
- Experience chronic illnesses like diabetes, heart disease, or cancer
All of these factors make seniors more susceptible to blood clots. That’s why prevention is so important, especially when support is available from facilities like Northern Heart Hospital, which specializes in senior vascular care.
The Most Common Types of Blood Clots in Seniors
Blood clots can strike in various parts of the body. Each type has different signs, risks, and prevention strategies.
Deep Vein Thrombosis (DVT)
This is the big one. DVT usually forms in the legs and is especially dangerous because the clot can break loose and travel to the lungs.
Common triggers:
- Long periods of bed rest
- Extended flights or car rides
- Surgery or injury
Symptoms: Leg pain, swelling, redness, and warmth — usually in one leg.
Pulmonary Embolism (PE)
This happens when a clot (often from DVT) moves to the lungs. It’s a medical emergency.
Symptoms include:
- Sudden shortness of breath
- Chest pain
- Rapid heartbeat
Arterial Thrombosis
This is when a clot forms in an artery, cutting off blood to the heart or brain — leading to heart attack or stroke.
This is more common in seniors with high blood pressure, high cholesterol, or a history of smoking.
Warning Signs You Should Never Ignore
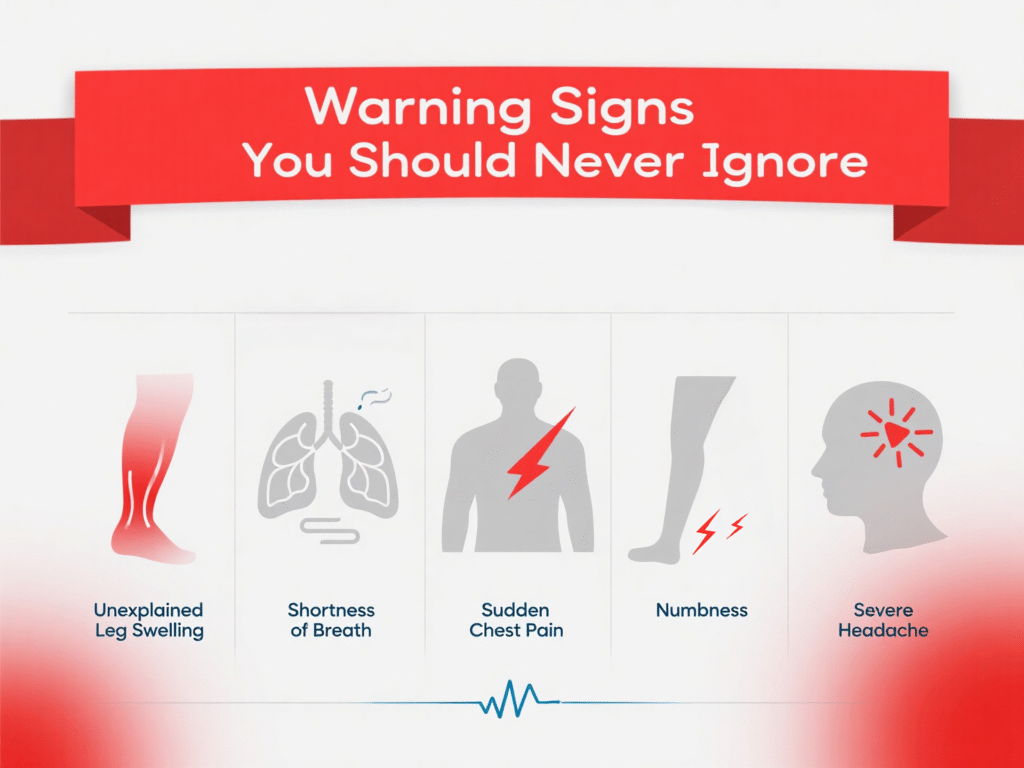
Early detection can be lifesaving. Watch for:
- Unexplained leg swelling or tenderness
- Shortness of breath
- Sudden chest pain
- Arm or leg numbness
- Severe headaches
If any of these signs appear, get help immediately. Hospitals like Northern Heart Hospital are equipped to assess and treat blood clots promptly.
The Role of Movement in Clot Prevention
Movement keeps your blood flowing like a smooth stream, not a stagnant pond.
Easy Daily Exercises for Seniors
You don’t need to run a marathon. Gentle movements can work wonders:
- Leg lifts while sitting
- Slow walking around the room every hour
- Ankle circles
- Chair yoga
These low-impact activities help keep blood from pooling in the legs.
The Danger of Prolonged Sitting
Sitting for long periods — even in your favorite recliner — increases clot risk. Set a timer to get up every 30–60 minutes. Stretch, move, breathe.
It’s a small act that prevents a big problem.
Staying Hydrated: The Overlooked Solution
Thick blood clots more easily — and dehydration thickens your blood. Seniors often don’t feel thirst as strongly, so it’s easy to forget.
Tips to stay hydrated:
- Keep a water bottle nearby
- Drink herbal teas or diluted juice
- Add hydration reminders to your daily routine
Even mild dehydration increases clot risk. So drink up!
Diet Tips: Foods That Help or Hurt
Your plate can be your prescription or your poison when it comes to clot prevention.
Foods That Thin the Blood Naturally
Certain foods are natural blood-thinners. Include these in your daily diet:
- Garlic
- Ginger
- Turmeric
- Salmon (rich in omega-3)
- Green leafy vegetables (spinach, kale)
Note: If you’re on blood-thinning meds, talk to your doctor about how these foods interact.
Foods to Avoid
Some foods increase clotting or interfere with medications:
- Processed meats
- Fried foods
- Excess sugar and salt
- High-vitamin K foods like liver (if you’re on warfarin)
A registered dietitian at Northern Heart Hospital can help tailor a diet that fits both your medication and lifestyle.
Medications and Their Role in Prevention
Doctors often prescribe blood thinners to elderly patients at risk. These include:
- Warfarin
- Heparin
- DOACs like Eliquis or Xarelto
These medications reduce your blood’s ability to clot. But be cautious — dosage and timing are critical. Too much can cause bleeding, too little can lead to clots.
Always take medications exactly as prescribed and report any side effects to your doctor.
Compression Stockings and Assistive Devices
Compression stockings work by gently squeezing your legs to promote blood flow. They’re especially helpful if:
- You sit for long periods
- You’re recovering from surgery
- You’ve had DVT before
Assistive devices like walkers also encourage movement, which helps blood flow naturally. Staff at Northern Heart Hospital can help assess and recommend the best options.
Preventive Screening and Regular Check-Ups
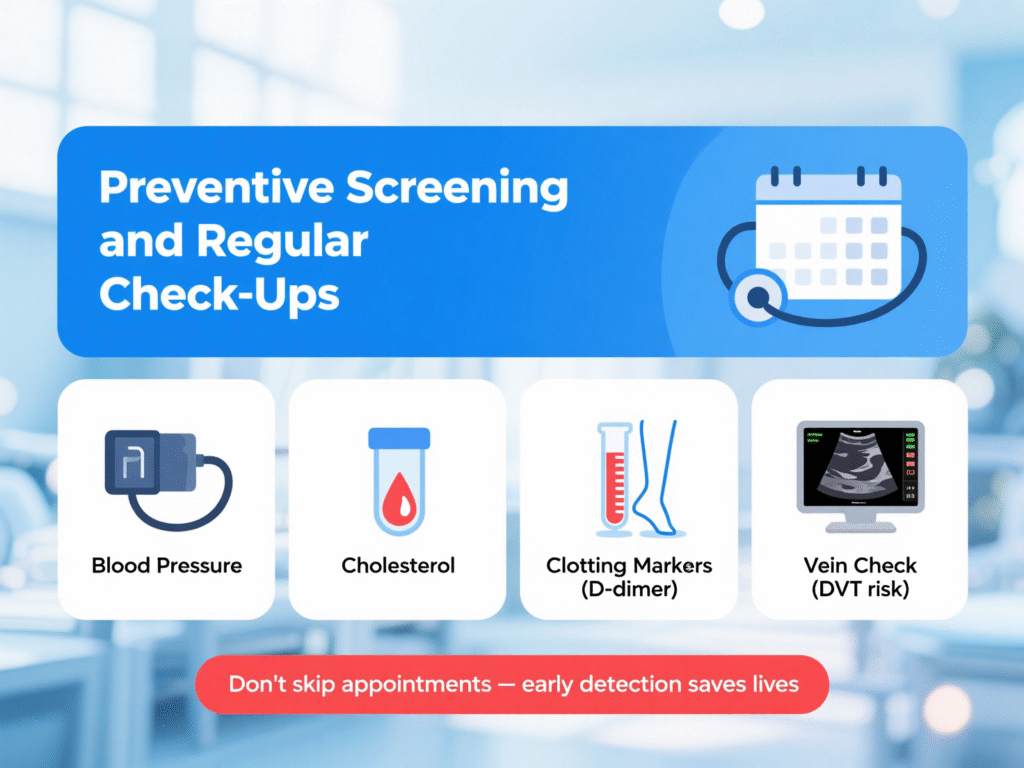
You can’t fix what you don’t know. Seniors should undergo regular screenings for:
- Blood pressure
- Cholesterol
- Blood clotting markers (like D-dimer tests)
- Ultrasound for leg veins (if there’s swelling or risk of DVT)
Don’t skip appointments. Regular monitoring helps catch problems before they become emergencies.
Post-Surgery Clot Prevention
Surgery is a major trigger for clots in older adults. That’s why post-op care plans often include:
- Blood-thinning medications
- Early mobilization (getting out of bed within 24 hours)
- Compression devices on the legs
Talk to your care team before and after surgery to build a strong prevention plan. The recovery teams at Northern Heart Hospital specialize in this kind of care.
Travel Tips for Seniors at Risk of Clots
Planning a trip? Keep these tips in mind:
- Wear loose clothing
- Walk the aisle or stretch every hour
- Stay hydrated (avoid alcohol)
- Use compression socks on long flights
- Carry essential medications in your carry-on
Long periods of immobility — like sitting in a plane seat — can silently trigger clots.
When to Seek Medical Help Immediately
Don’t second-guess serious symptoms. Call a doctor or go to the ER if you experience:
- Unexplained leg swelling or redness
- Sudden chest pain
- Trouble breathing
- Vision changes or confusion
- Arm or leg weakness
The faster you act, the better the outcome.
Conclusion: Taking Small Steps Toward Big Protection
Preventing blood clots doesn’t require massive lifestyle changes. It’s the little things, done consistently, that keep the blood flowing safely.
Whether you’re a senior, caregiver, or concerned loved one — the message is the same: stay active, stay hydrated, eat well, and know the signs.
And don’t hesitate to seek expert care from trusted institutions like Northern Heart Hospital, where prevention and compassion go hand in hand.
FAQs
1. Can blood clots go away on their own?
Small clots may dissolve naturally, but many require medication. Never ignore symptoms — it’s not worth the risk.
2. Are compression stockings uncomfortable?
At first, maybe. But with proper fitting and use, most people find them manageable and even comforting.
3. What medications help prevent blood clots?
Warfarin, Eliquis, Xarelto, and Heparin are common. Your doctor will recommend based on your health and lifestyle.
4. Can diet alone prevent blood clots?
Diet helps — especially anti-inflammatory foods — but it should be combined with movement, hydration, and medical oversight.
5. How often should seniors be screened for clot risk?
At least once a year — or more often if they’ve had clots before or have chronic health conditions.
