What You Need to Know About Hypertension in Middle Age
Middle age is often described as a balancing act—juggling work, family, and personal health. Yet, it’s also the time when your body begins sending subtle warnings. One of the most common, yet easily overlooked, is hypertension, also known as high blood pressure. Understanding how it develops, why it worsens with age, and what you can do about it can make all the difference in preventing serious health complications down the road.
Understanding Hypertension: The Silent Killer
Hypertension is often referred to as the “silent killer” because it usually has no noticeable symptoms until significant damage has already been done. Imagine water pressure in your home’s pipes. If the pressure is consistently too high, over time the pipes weaken, leak, or even burst. The same principle applies to your blood vessels. Constantly elevated blood pressure weakens artery walls and forces your heart to work harder, which can eventually lead to heart attacks, strokes, and organ failure if left unchecked.
Why Middle Age is the Turning Point for Blood Pressure
By the time you hit your 40s or 50s, your body has already undergone years of wear and tear. Arteries naturally lose some of their flexibility, making it harder for blood to flow smoothly. This stiffening effect, combined with lifestyle factors like diet, stress, and inactivity, creates the perfect storm for developing hypertension. Middle age is the pivotal moment when preventative action matters most, because this is when your risk for heart disease, kidney problems, and stroke begins to climb sharply.
Common Risk Factors of Hypertension in Middle Age
Hypertension doesn’t appear out of thin air—it’s the result of multiple factors building up over time.
Genetic Influence and Family History
If your parents or siblings struggle with high blood pressure, chances are you may too. Genetics play a significant role, but it’s not destiny—you can reduce the risk with the right lifestyle choices.
Lifestyle Habits that Add Pressure
Smoking, excessive alcohol, and eating processed or salty foods are direct contributors to hypertension. Over time, these habits create chronic stress on your cardiovascular system, making high blood pressure harder to control.
Stress and Its Hidden Effects
Daily stress may feel like just part of modern life, but when your body is constantly producing stress hormones, your blood vessels constrict, heart rate rises, and pressure builds. Over the years, unmanaged stress becomes a silent driver of hypertension.
Early Symptoms You Shouldn’t Ignore
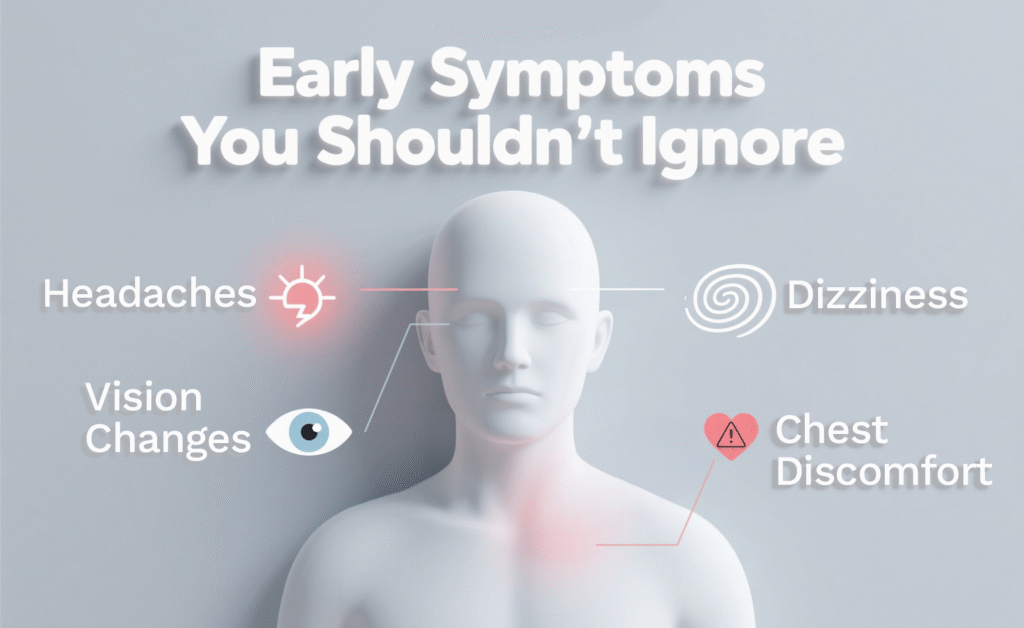
While hypertension is often symptomless, certain warning signs may occasionally show up. Frequent headaches, unexplained dizziness, blurred vision, or chest discomfort could be signals that your blood pressure is creeping up. Don’t brush these off—treat them as a red flag to get checked.
How Hypertension Affects Your Body Over Time
High blood pressure isn’t just about numbers—it’s about the damage those numbers cause day after day.
Impact on the Heart and Arteries
The heart has to pump harder, which thickens its muscle walls and increases the risk of heart failure. Blood vessels also stiffen and clog more easily, raising the likelihood of heart attacks.
Damage to Kidneys and Eyes
Your kidneys filter toxins and excess fluid. Hypertension gradually damages their delicate filters, leading to kidney disease. Similarly, tiny vessels in the eyes weaken, causing vision loss or even blindness.
Cognitive Decline and Stroke Risk
Consistently high blood pressure reduces blood flow to the brain, impairing memory and concentration. Over time, the risk of strokes and dementia rises significantly.
Diagnostic Tests for Detecting Hypertension
A simple blood pressure reading is the first step, but doctors may recommend more tests—such as blood work, urine tests, or ECGs—to see if your organs are already affected. Regular check-ups at trusted facilities like Northern Heart Hospital can catch problems before they escalate.
Practical Lifestyle Changes to Manage Blood Pressure
Managing hypertension doesn’t always begin with medication. Small, consistent lifestyle changes can significantly lower blood pressure.
Eating Smart: Heart-Friendly Foods
Think of food as fuel. Replacing salty snacks with fruits, vegetables, whole grains, and lean proteins helps your arteries stay flexible. Foods rich in potassium, like bananas and spinach, balance out sodium levels and naturally lower pressure.
Staying Active Without Overdoing It
You don’t need to become a marathon runner to protect your heart. Even brisk walking for 30 minutes daily can lower blood pressure and improve circulation. Exercise is like oiling your car engine—it keeps things running smoothly.
Weight Management and Its Importance
Excess weight forces your heart to work harder. Shedding even 5–10% of your body weight can have a dramatic impact on lowering hypertension risks.
The Role of Stress Reduction and Sleep
Stress reduction techniques like deep breathing, meditation, or yoga can lower blood pressure by calming the nervous system. Just as important is sleep—consistent, quality rest allows your body to repair itself. Poor sleep, on the other hand, raises stress hormones and worsens hypertension.
Medications and When They Become Necessary
Sometimes, lifestyle changes alone aren’t enough. Doctors may prescribe medications like ACE inhibitors, beta-blockers, or diuretics to control pressure. The key is adherence—taking them regularly as prescribed prevents dangerous spikes. Never stop or change doses without consulting your doctor.
Regular Check-Ups and Monitoring Progress
Hypertension requires ongoing attention, not just a one-time fix. Home blood pressure monitors make it easy to track your numbers daily. Routine visits to clinics such as Northern Heart Hospital ensure professional monitoring and adjustments if needed.
How Middle-Aged Adults Can Stay Motivated for Long-Term Heart Health
It’s easy to feel discouraged when changes don’t bring instant results. Think of heart health as a marathon, not a sprint. Setting small, achievable goals—like reducing salt intake or walking three times a week—keeps motivation high. Celebrating little wins makes the journey sustainable.
When to Seek Professional Help from Specialists
If lifestyle adjustments and initial treatments aren’t controlling your numbers, it may be time to see a cardiologist or hypertension specialist. Facilities like Northern Heart Hospital provide advanced testing and personalized treatment plans for better outcomes.
Conclusion
Hypertension in middle age may be common, but it’s far from inevitable. With the right knowledge, lifestyle adjustments, and medical guidance, you can keep your blood pressure under control and safeguard your long-term health. The key is consistency—small daily efforts add up to lifelong benefits.
FAQs
Q1: Can hypertension in middle age be reversed?
Yes, in many cases early hypertension can be managed or even reversed with lifestyle changes like diet, exercise, and weight control.
Q2: How often should I check my blood pressure after age 40?
At least once a year during routine check-ups, or more frequently if you already have elevated readings.
Q3: Is hypertension more common in men or women during middle age?
Men tend to develop hypertension earlier, but women’s risk rises significantly after menopause.
Q4: Can stress alone cause hypertension?
Chronic stress doesn’t always cause hypertension on its own, but it contributes significantly by tightening blood vessels and raising heart rate.
Q5: What’s the best exercise for lowering blood pressure?
Aerobic activities like brisk walking, cycling, and swimming are most effective, especially when done regularly.
