The Step-by-Step Process of Getting a Carotid Stent
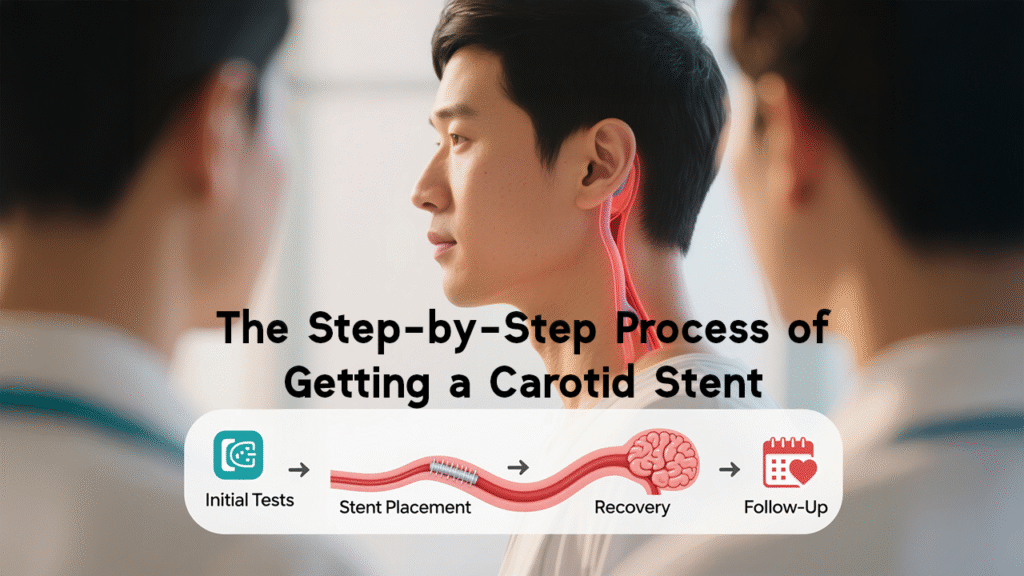
Getting a carotid stent is a major step toward preventing future strokes and protecting brain health. In plain language, the procedure opens up a narrowed neck artery so oxygen rich blood can reach your brain consistently. If your doctor recommended a carotid stent, you probably have a lot of questions. This article walks you through the whole process, from the first tests to long term follow up, using clear explanations and helpful examples so you know what to expect.
Why Carotid Stenting Matters
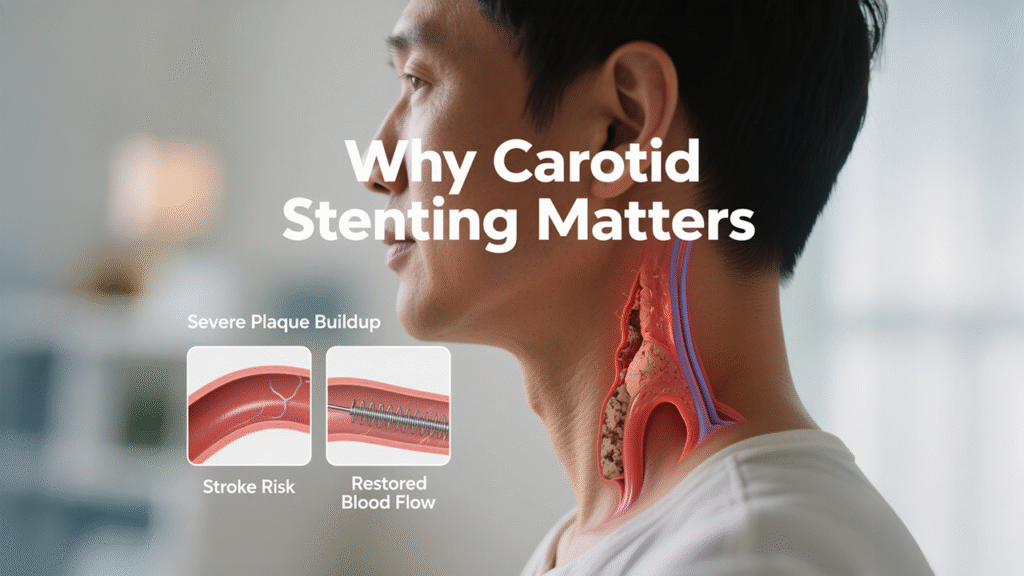
Carotid stenting is offered when the carotid arteries are narrowed enough to increase stroke risk. For example, if an imaging test shows a severe plaque buildup and you have symptoms like brief weakness or slurred speech, your care team may recommend stenting to lower the chance of a disabling stroke. That is the practical reason this procedure exists, and that is what we will unpack step by step.
Understanding the Carotid Arteries
The carotid arteries run along each side of your neck. They are the main highways that deliver oxygen rich blood from your heart to your brain. If these highways become narrowed, the brain can be starved of oxygen temporarily or permanently. Think of it like a water pipe that gradually gets clogged with sediment, reducing flow to the tap at the other end.
What Causes Carotid Artery Narrowing
Most narrowing is caused by plaque buildup inside the artery wall. Plaque is a mixture of cholesterol, calcium, inflammatory cells and scar tissue that gradually accumulates.
Atherosclerosis and Plaque Formation
Atherosclerosis develops over years. Initially the artery walls thicken, then soft fatty deposits form, and later the deposits harden. A plaque may stay stable for a long time or it may ulcerate and release debris that can travel to the brain and cause a blockage.
Who Is at Risk
People with high blood pressure, high cholesterol, diabetes, a history of smoking, or a family history of vascular disease are at higher risk. Older adults are more susceptible because plaque accumulates with age. Recognizing risk factors helps doctors decide who needs testing.
Signs and Symptoms That Lead to Evaluation
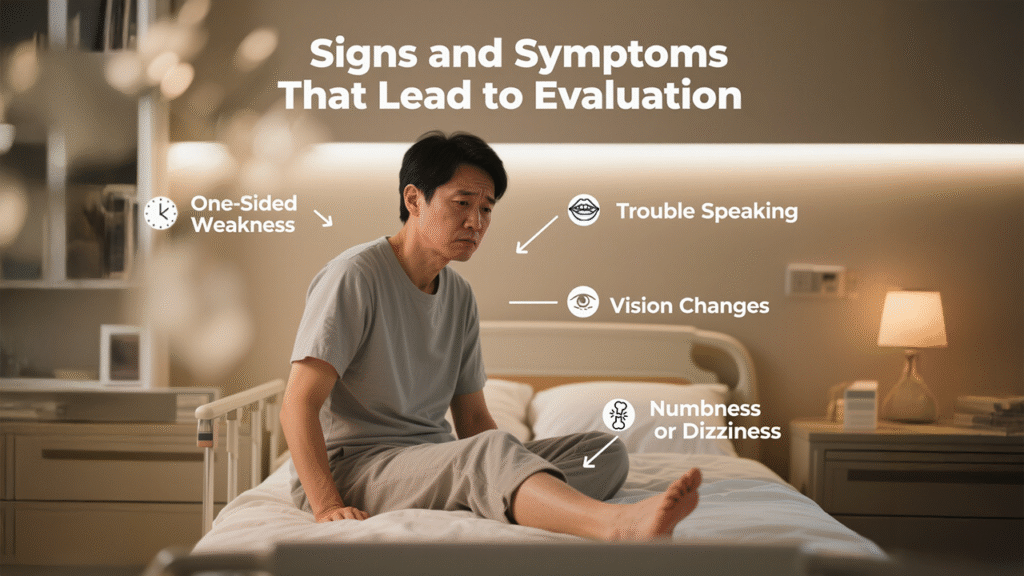
Symptoms that prompt evaluation include sudden weakness on one side, sudden trouble speaking, sudden vision changes in one eye, or brief spells of numbness or dizziness. These may be transient ischemic attacks, which are warning signals that the underlying carotid artery may be unsafe.
How Doctors Confirm the Problem
Imaging tests are essential to measure the degree of narrowing and to plan a safe treatment.
Carotid Ultrasound
Carotid ultrasound uses sound waves to show plaque and estimate how much the artery is narrowed. It is non invasive and often the first test ordered.
CT Angiography and MR Angiography
CT angiography and MR angiography provide clearer, three dimensional pictures of the artery, including the length and shape of the blockage. These scans help doctors plan the best approach for treatment.
Digital Subtraction Angiography
Digital subtraction angiography is an invasive but gold standard test that shows tiny details of the artery. It is sometimes performed right before the stenting procedure so the interventional team can map the artery precisely.
When Is a Carotid Stent Recommended
A stent may be recommended if the narrowing is severe, for example over 50 percent in symptomatic patients, and if open surgery carries high risk. Physicians weigh individual factors, such as age, heart and lung function, anatomic considerations, and previous neck operations, to decide whether stenting is the safer option.
Step 1: Pre-Procedure Evaluation and Decision Making
Before any procedure, a thorough evaluation ensures that stenting is the right choice for you.
Medical History and Risk Assessment
Your team reviews your overall health, medications, allergies, and prior procedures. They also assess stroke risk and whether you had recent transient ischemic attacks.
Medication Review and Optimization
Some medications may need to be adjusted. For example, your doctor will usually start or continue antiplatelet therapy, which helps prevent clots during and after the stent placement. Your cardiologist or neurologist will tailor a medication plan specific to your needs.
Step 2: Preparing for the Procedure
Proper preparation reduces complications and smooths recovery.
Fasting, Consent, and Practical Logistics
You will receive clear instructions on when to stop eating and drinking, typically several hours before the procedure. You will sign informed consent after the team explains risks and benefits. Arrange a ride home and a comfortable place to recover after discharge.
Pre-procedure Medications and Imaging Review
Your team reviews all imaging and blood tests, which may include kidney function, and coagulation status. If contrast dye is required, kidney function is checked to ensure safe use.
Step 3: The Procedure Day — Arrival and Anesthesia
On the day, you arrive at the hospital, change into a gown, and meet the team.
Local Sedation versus General Anesthesia
Carotid stents can be performed with moderate sedation and local numbing at the catheter entry site. You stay awake but relaxed. In some cases general anesthesia is used based on medical considerations. The team will explain what to expect.
Step 4: Catheter Navigation and Embolic Protection
The interventionalist accesses the arterial system, most commonly through the femoral artery in the groin, and advances a guidewire and catheter to the carotid artery.
Guidewire and Catheter Techniques
Using continuous X ray guidance, the team navigates the catheter up to the neck. This navigation is precise and gentle so as to avoid disturbing the plaque before protective measures are in place.
Embolic Protection Devices, explained with an example
An embolic protection device is like a tiny filter placed downstream from the blockage. For example, if a small fragment of plaque dislodges during stent placement, the filter catches it, preventing it from traveling to the brain. This simple example helps explain why protection devices are standard in most procedures.
Step 5: Balloon Angioplasty and Stent Deployment
Once protection is in place, the team performs balloon angioplasty and then deploys the stent.
Types of Stents and how they work
A stent is a small mesh tube that expands to support the artery wall. Some stents expand by a balloon inside them, others are self expanding. The stent holds the artery open and restores a smoother flow of blood, reducing turbulent zones where clots tend to form.
Step 6: Immediate Post-Deployment Checks and Recovery
After placement, imaging confirms stent position and blood flow improvement.
Imaging confirmation and neurological monitoring
Immediate angiography and neurological checks ensure that the brain is receiving improved blood supply and that there are no immediate complications such as a new neurological deficit. The team monitors your blood pressure closely, because blood pressure swings can stress the stented area.
Step 7: In-Hospital Recovery and Observation
You will be observed for several hours up to overnight depending on your condition.
Doctors and nurses monitor the catheter insertion site, pulses in the wrist and ankle, and neurological status. Early mobilization and walking are encouraged to reduce the risk of complications like blood clots.
Step 8: Discharge, Medications, and Early Follow-Up
Most patients go home the next day, once stable.
You will continue antiplatelet medications for a prescribed period, often a combination of aspirin and another agent. The exact regimen depends on your physician. You will have a follow up visit within a few weeks and an ultrasound to confirm the stent remains open.
Long-Term Follow-Up and Lifestyle Changes
Long term success depends on medication adherence and lifestyle.
Control blood pressure and cholesterol with medication and diet. Stop smoking. Exercise regularly. These measures reduce the chance of new plaque forming and improve overall vascular health. Regular medical follow up and periodic imaging help detect any problems early, when they are easiest to treat.
Benefits and Expected Outcomes
Carotid stenting usually reduces the risk of future stroke by restoring smooth blood flow. Many patients report better cognitive clarity and reduced fatigue after recovery. The minimally invasive nature of the procedure allows shorter hospital stays and quicker return to daily life.
Possible Risks and How They Are Minimized
Risks include bleeding at the catheter site, allergic reaction to contrast dye, a small risk of stroke during the procedure, and rarely infection. Experienced teams minimize these risks by careful patient selection, meticulous technique, and the routine use of protection devices.
Choosing the Right Hospital and Team
Selecting a hospital with experienced surgeon and strong multidisciplinary support matters. Look for centers that perform carotid stenting frequently and have protocols for rapid diagnosis and complication management.
Why Patients Choose Northern Heart Hospital
Patients often choose Northern Heart Hospital because it offers experienced operators, modern imaging suites, and coordinated care between neurology, cardiology, and vascular surgery. That multidisciplinary approach helps ensure the safest pathway from diagnosis to recovery.
Conclusion
The process of getting a carotid stent involves careful evaluation, precise procedure steps, and committed follow up. When performed by an experienced team, the procedure can meaningfully reduce stroke risk and help you return to normal life quickly. Know the steps, ask questions, and work with your care team to get the best possible outcome for your brain health.
FAQs
1. How long does the carotid stent procedure take?
Typically, the procedure lasts one to two hours, but total time at the hospital may be longer due to preparation and recovery.
2. Will I be awake during the procedure?
Most patients receive local anesthesia and sedation, so you are usually awake but comfortable. In some cases general anesthesia is used.
3. How soon can I return to work and normal activities?
Many people resume light activities within a few days and return to normal work within one to two weeks, depending on individual recovery.
4. Are carotid stents permanent?
Yes, the stent remains in place permanently. Regular follow up and healthy lifestyle choices help maintain long term success.
5. What warning signs should make me call my doctor after discharge?
Contact your team if you experience new weakness, slurred speech, sudden vision changes, severe headache, fever, increasing pain or swelling at the insertion site, or bleeding that will not stop.
6. When to Consider a Carotid Stent Consultation
If you are experiencing any of the symptoms mentioned above, please arrange an appointment with Dr. Edward Choke Tieng Chek for an evaluation and discussion on whether a carotid stent is the right treatment option for you.
