The heart is one of the most vital organs in the body, performing the crucial function of pumping blood throughout the entire circulatory system. It is responsible for delivering oxygen and nutrients to tissues and removing metabolic waste products. When the heart muscle becomes damaged or weak, its ability to perform these tasks is compromised, leading to cardiomyopathy. Cardiomyopathy refers to a group of diseases that affect the heart muscle and can significantly impact a person’s overall health and quality of life. This condition can lead to heart failure, arrhythmias (irregular heartbeats), and even sudden cardiac arrest in severe cases.
At Northern Heart Hospital, we are committed to providing vital information and expert care for those facing cardiomyopathy. We understand the importance of early diagnosis and effective treatment, which is why our state-of-the-art facilities and comprehensive services are designed to address all aspects of this condition. From advanced diagnostic tools to personalised treatment plans, our team of specialists is dedicated to helping you manage cardiomyopathy with the best care possible, so you can maintain a healthy heart and a fulfilling life.
What is Cardiomyopathy?
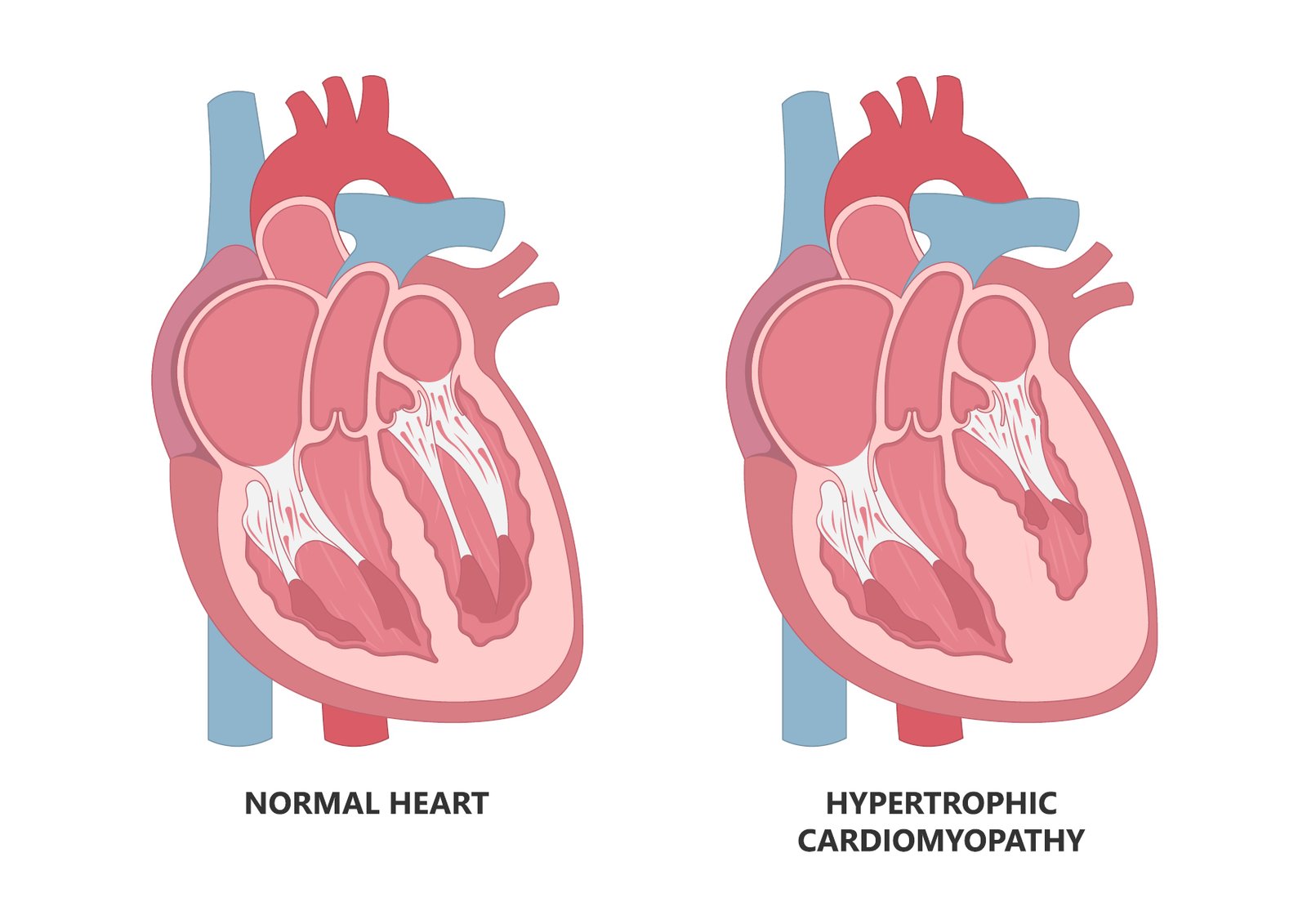
Cardiomyopathy is not just one condition, but rather a term used to describe a range of diseases that directly affect the heart muscle. There are various forms of cardiomyopathy, each with its own underlying causes, symptoms, and treatment strategies. Understanding these different types is important for both patients and healthcare providers, as the management and prognosis of each type can differ significantly.
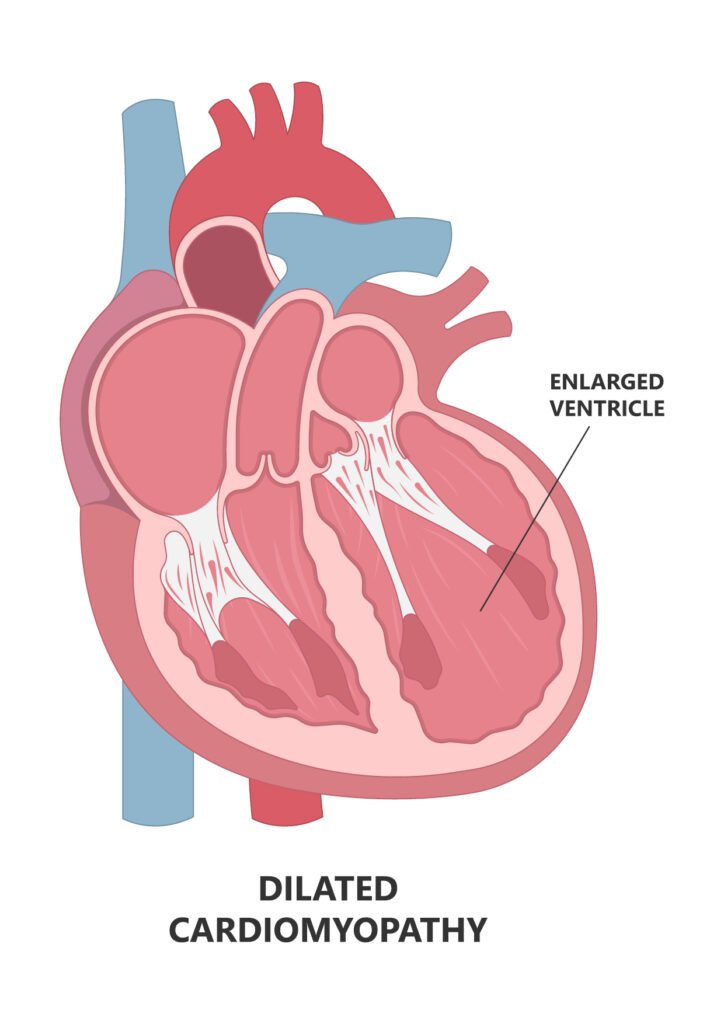
Dilated Cardiomyopathy (DCM) is one of the most common types of cardiomyopathy. It occurs when the heart’s chambers become enlarged (dilated) and the heart muscle becomes weak. As the heart becomes larger, its ability to contract and pump blood decreases, leading to a condition known as heart failure. Symptoms of DCM can include fatigue, swelling of the legs and abdomen, and shortness of breath. This type of cardiomyopathy can affect people of all ages and is sometimes linked to genetic factors or other conditions like high blood pressure or viral infections.
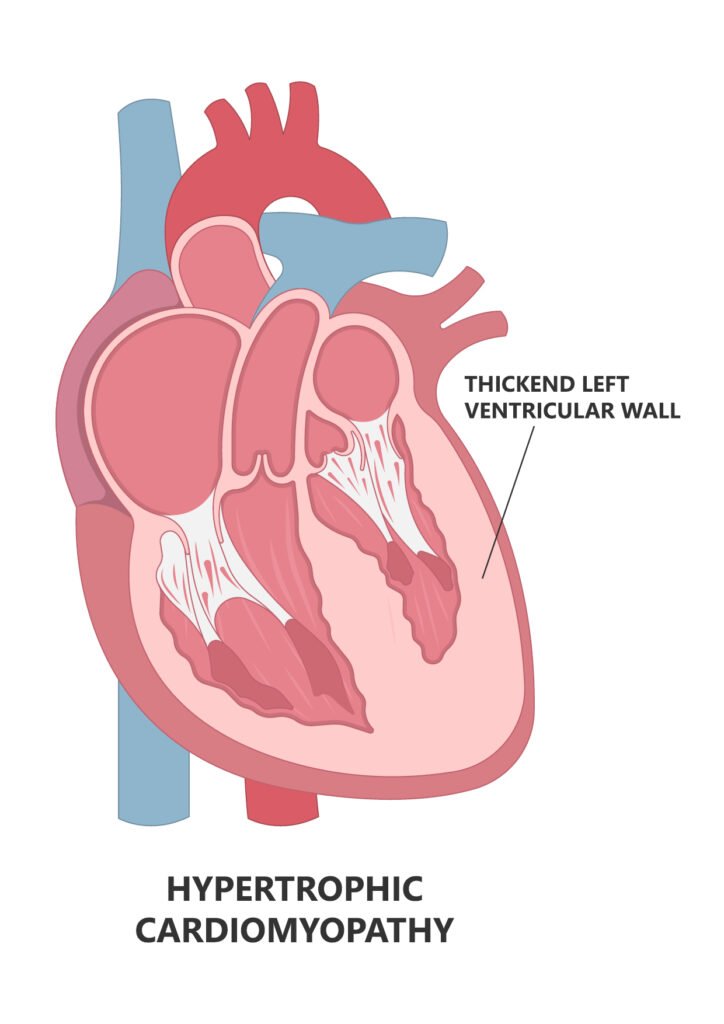
Hypertrophic Cardiomyopathy (HCM) is a condition in which the heart muscle thickens abnormally, often in the left ventricle, which can obstruct blood flow and reduce the heart’s efficiency. HCM is a genetic condition and is commonly inherited, which means it can run in families. In many cases, individuals with HCM may not experience symptoms until later in life. However, it can cause chest pain, fainting, palpitations, and, in severe cases, sudden cardiac death, especially in young athletes. Diagnosis is often made through an echocardiogram or genetic testing, as early detection is critical in managing this condition.
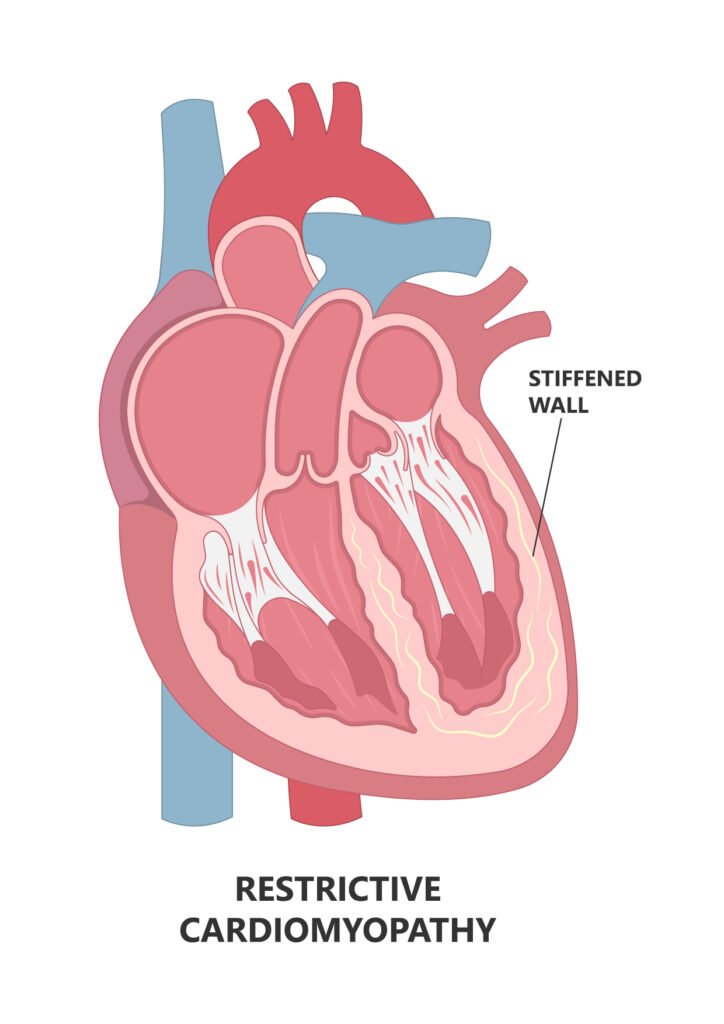
Restrictive Cardiomyopathy (RCM) is characterised by stiffening of the heart muscle, which makes it harder for the heart to fill with blood. Unlike other types of cardiomyopathy, the heart’s chambers may not dilate, but the impaired filling can lead to reduced blood flow and symptoms like swelling, breathlessness, and fatigue. RCM is often a result of other systemic conditions such as amyloidosis or other forms of heart muscle infiltration.
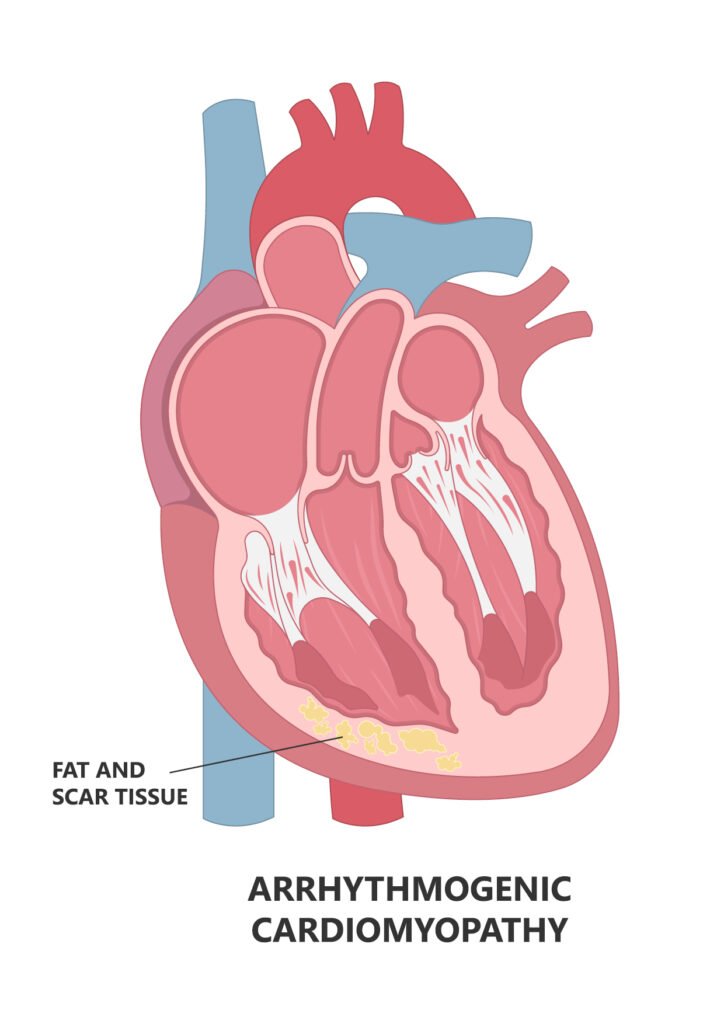
Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC) is a rare condition that causes the replacement of heart muscle in the right ventricle with fatty or fibrous tissue, leading to abnormal heart rhythms and an increased risk of sudden cardiac death. ARVC typically presents with symptoms like palpitations, dizziness, and fainting. Because of the risk of sudden cardiac arrest, individuals diagnosed with ARVC may require an implantable cardioverter defibrillator (ICD) to monitor and manage arrhythmias.
What Causes Cardiomyopathy?
Cardiomyopathy can be caused by a variety of factors, and often, more than one factor is at play. Some of the most common causes include:
- Genetic factors: Many forms of cardiomyopathy, especially hypertrophic cardiomyopathy, are inherited. Individuals with a family history of cardiomyopathy should be aware of the genetic component and consider getting screened. Genetic counselling may also be helpful for individuals with a known family history.
- High blood pressure (Hypertension): One of the leading causes of cardiomyopathy is prolonged high blood pressure. Over time, untreated high blood pressure puts a strain on the heart, making it work harder to pump blood. This added pressure can weaken the heart muscle, leading to dilated cardiomyopathy.
- Viral infections: Some viral infections, especially those that affect the heart, can lead to a condition called myocarditis, which causes inflammation and damage to the heart muscle. In some cases, myocarditis can progress to cardiomyopathy, particularly in individuals with weakened immune systems.
- Alcohol and drug use: Chronic alcohol abuse is a significant risk factor for developing alcoholic cardiomyopathy. Alcohol is toxic to the heart muscle, and over time, excessive drinking can lead to a weakened heart that struggles to pump blood effectively. Similarly, some recreational drugs, such as cocaine, can have toxic effects on the heart and contribute to cardiomyopathy.
- Other medical conditions: Diabetes, thyroid disorders, autoimmune diseases, and certain metabolic conditions can all increase the risk of developing cardiomyopathy. Conditions like lupus, rheumatoid arthritis, and scleroderma can cause inflammation in the heart muscle, while uncontrolled diabetes can contribute to the development of heart disease.
- Medications and cancer treatments: Certain medications, particularly chemotherapy drugs, can damage the heart muscle. Patients undergoing cancer treatment should discuss the potential risks with their oncologists, as some chemotherapy drugs are known to cause heart problems. In addition, radiation therapy targeted at the chest can also increase the risk of cardiomyopathy.
- Nutritional deficiencies: Severe vitamin or mineral deficiencies, especially those related to thiamine (vitamin B1), can contribute to cardiomyopathy. Thiamine deficiency can cause a form of heart disease known as wet beriberi, which leads to heart enlargement and failure.
Symptoms of Cardiomyopathy
Cardiomyopathy can be asymptomatic in its early stages, particularly in conditions like hypertrophic cardiomyopathy, where symptoms may not appear until adulthood. However, as the disease progresses, various symptoms may develop, including:
- Fatigue: One of the most common symptoms of cardiomyopathy is excessive tiredness, as the weakened heart cannot pump enough blood to meet the body’s oxygen needs.
- Breathlessness: Shortness of breath often occurs because the heart is not pumping efficiently, leading to fluid buildup in the lungs (pulmonary oedema). This can make even mild physical activity difficult and may worsen over time.
- Swelling (Oedema): Swelling in the legs, ankles, feet, and abdomen occurs when the heart is unable to effectively circulate blood. This fluid retention can be a sign of worsening heart failure.
- Chest pain: While chest pain is most commonly associated with coronary artery disease, individuals with hypertrophic cardiomyopathy may also experience chest pain due to the thickened heart muscle restricting blood flow.
- Irregular heartbeats (Arrhythmias): A common symptom in individuals with cardiomyopathy is arrhythmias, which can manifest as palpitations or irregular, racing heartbeats. In severe cases, these arrhythmias may lead to fainting or sudden cardiac arrest.
- Dizziness or fainting: Individuals with cardiomyopathy may feel light-headed or dizzy, especially when standing up quickly, as the heart’s reduced pumping capacity can cause a temporary drop in blood pressure.
Diagnosing Cardiomyopathy
Early diagnosis is essential for effective management of cardiomyopathy. Doctors typically use a combination of imaging tests and diagnostic procedures to assess the heart’s function and structure:
- Echocardiogram: This non-invasive test uses ultrasound waves to create images of the heart’s chambers, valves, and blood flow. It helps doctors identify enlarged or thickened heart walls, abnormal heart function, and fluid buildup.
- Electrocardiogram (ECG): An ECG records the electrical activity of the heart and can detect arrhythmias, which are often present in individuals with cardiomyopathy.
- Cardiac MRI: A cardiac MRI provides detailed images of the heart and is particularly useful for diagnosing conditions like arrhythmogenic right ventricular cardiomyopathy (ARVC) and other forms of structural heart disease.
- Blood tests: Blood tests can help identify underlying conditions, such as infections, inflammation, or hormonal imbalances, that may contribute to cardiomyopathy.
- Genetic testing: For patients with a family history of cardiomyopathy, genetic testing may be performed to identify mutations in the genes associated with the disease.
Treatment and Management of Cardiomyopathy
The treatment of cardiomyopathy depends on the type, severity, and underlying causes of the condition. While some forms of cardiomyopathy can be managed with medications and lifestyle changes, others may require more invasive treatments.
- Medications: Common medications prescribed to treat cardiomyopathy include:
- Beta-blockers to reduce the heart rate and improve blood flow.
- ACE inhibitors to help relax blood vessels and reduce the strain on the heart.
- Diuretics to reduce fluid retention and alleviate swelling.
- Anti-arrhythmic medications to help control abnormal heart rhythms.
- Medical devices: Patients with cardiomyopathy may require implantable devices to help regulate their heart’s function, including:
- Pacemakers to maintain a regular heart rhythm.
- Implantable cardioverter defibrillators (ICDs) to prevent sudden cardiac arrest caused by arrhythmias.
- Surgery: In certain cases, surgery may be necessary, such as:
- Septal Myectomy: A procedure used for hypertrophic cardiomyopathy to remove excess thickened heart tissue and improve blood flow.
- Heart Transplantation: For patients with advanced heart failure, a heart transplant may be the only viable option.
- Lifestyle changes: Patients with cardiomyopathy should focus on maintaining a healthy lifestyle. This includes eating a balanced diet, exercising regularly (under medical supervision), avoiding smoking, limiting alcohol intake, and reducing stress.
- Monitoring: Regular follow-up visits with a healthcare provider are critical for managing cardiomyopathy and adjusting treatment plans as necessary.
Living with Cardiomyopathy
While cardiomyopathy is a serious condition, many people with the disease are able to lead fulfilling and active lives with the right management. With proper treatment, lifestyle changes, and regular monitoring, the progression of the disease can be slowed, and quality of life can be maintained.
Expert Care at Northern Heart Hospital
At Northern Heart Hospital, we offer cutting-edge care for individuals with cardiomyopathy. Our team of highly skilled cardiologists, specialists, and healthcare providers are committed to delivering personalised care, ensuring that each patient receives the best possible treatment for their condition. If you or a loved one is experiencing symptoms of cardiomyopathy, don’t hesitate to reach out for expert care. With the right treatment and support, it’s possible to manage the condition and live a heart-healthy life. Contact us today to begin your journey toward better heart health.
