Early Warning Signs of Artery Blockage in Legs
Blocked arteries are not just a heart problem. They can happen in your legs too, and when they do, it is called Peripheral Artery Disease (PAD). Left unchecked, this condition can lead to limb loss. The good news? Your body gives you early clues before things get serious. Let us explore these early signs and what to do about them.
Understanding Artery Blockage in Legs
Peripheral Artery Disease occurs when fatty deposits (plaques) build up in the arteries of your legs, restricting blood flow. Think of your arteries as garden hoses. When they get kinked or clogged, water (or in this case, blood) cannot flow freely. That can cause pain, weakness, and long-term damage.
What Causes Peripheral Artery Disease (PAD)?
PAD typically results from atherosclerosis, the same condition that causes heart attacks. Risk factors include smoking, high cholesterol, high blood pressure, diabetes, and age. People over 50, especially with a history of cardiovascular disease or diabetes, are more prone to developing PAD.
Why Early Detection Matters
Early diagnosis can prevent severe complications. If the blood supply is severely restricted for too long, tissues in the leg begin to die, potentially leading to amputations. Plus, PAD often coexists with coronary artery disease, so spotting it early may even help prevent heart problems down the line.
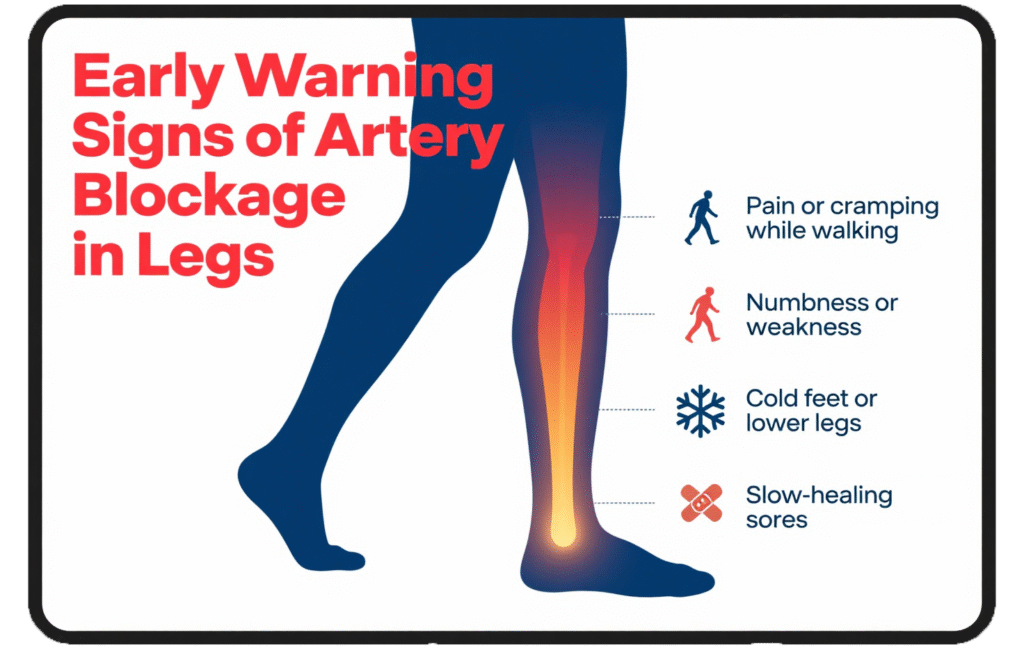
Common Early Symptoms to Watch For
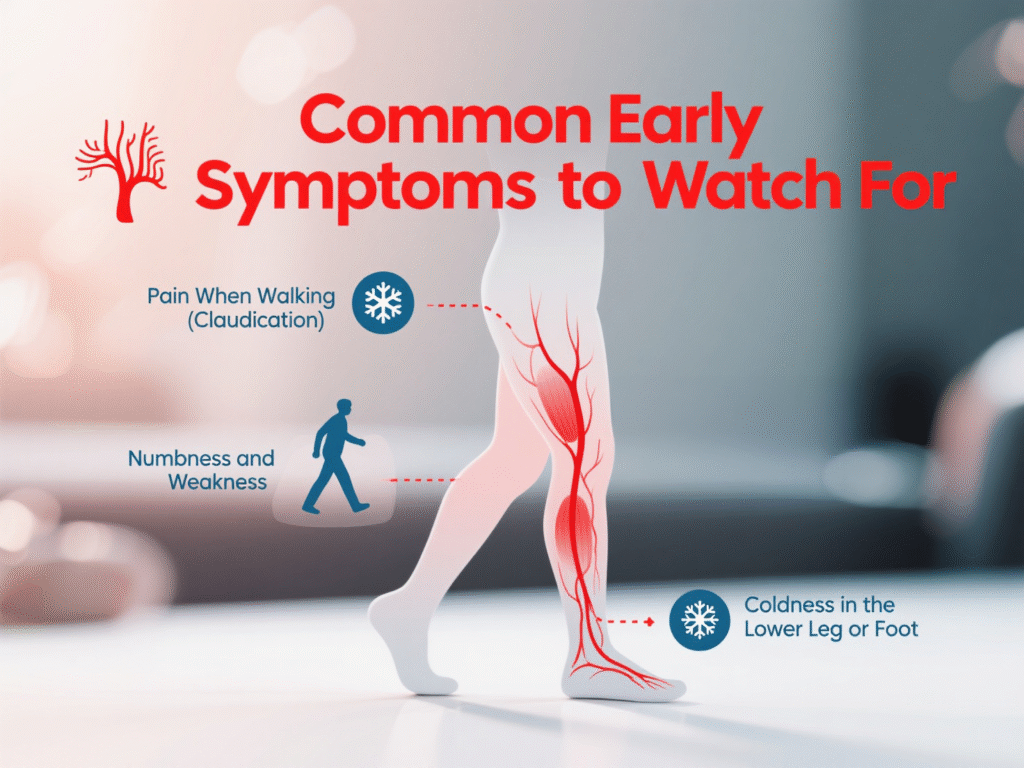
Pain When Walking (Claudication)
This is the most classic symptom. It feels like a cramp, tightness, or aching in the calf, thigh, or buttocks when walking. It usually disappears after rest and comes back during activity. Do not ignore this. It is your body’s cry for help.
Numbness and Weakness in the Legs
If your legs feel weak or “fall asleep” often, this could signal restricted circulation. These signs tend to worsen at night or after physical activity.
Coldness in the Lower Leg or Foot
One leg colder than the other? That is a red flag. Poor blood flow means that your tissues are not getting the warmth and oxygen they need.
Changes in Skin Color and Temperature
- Poor Wound Healing or Sores on Toes
Small cuts or sores on your toes, feet, or legs that take weeks to heal could point to PAD. Reduced blood flow means fewer nutrients and oxygen for repair.
- Slower Toenail or Hair Growth
You may not notice this immediately, but a lack of hair or slow-growing toenails can be silent signs of a circulation problem.
- Leg Fatigue Without Physical Activity
If your legs feel unusually heavy, tired, or restless even without walking, this could be due to limited blood reaching your muscles.
Less Obvious But Serious Signs
- Erectile Dysfunction in Men
Yes, PAD can affect more than just your legs. Erectile dysfunction, particularly in men under 60 with risk factors like diabetes or smoking, could be an early vascular warning.
- Weak Pulse in Legs or Feet
A healthcare provider may detect this during a physical exam. A weak or absent pulse in your feet is a strong indicator of restricted blood flow.
- Shiny, Tight, or Thin Skin on Legs
This may look like your skin is stretched tightly over the leg and has a glossy appearance. It is often a subtle yet telling sign of PAD.
When to See a Specialist
If you notice even one or two of these symptoms, it is time to see a vascular surgeon. You do not have to wait until it becomes unbearable. At Northern Heart Hospital, our specialists are trained to detect and treat PAD early, reducing your risk of complications.
How Artery Blockage Is Diagnosed
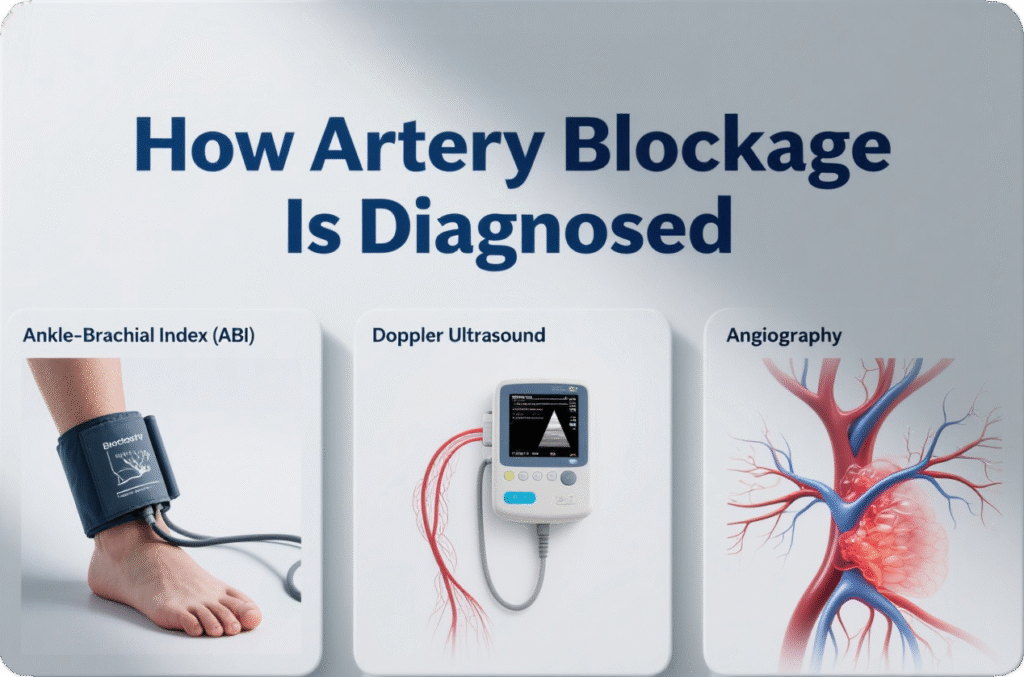
Doctors use several tests to confirm PAD:
- Ankle-Brachial Index (ABI): This painless test compares blood pressure in your ankles to that in your arms.
- Doppler Ultrasound: Provides images of blood flow in your leg arteries.
- Angiography: Uses dye and imaging to spot blockages.
These tests are available at Northern Heart Hospital, where advanced diagnostic tools help ensure accurate, early detection.
Treatment Options for Blocked Leg Arteries
Treatment depends on severity. Mild cases may only need lifestyle changes, while severe ones might require surgery.
Lifestyle Changes That Make a Difference
Quit Smoking and Manage Cholesterol
Smoking is PAD’s best friend. Quitting is non-negotiable. Combine that with lowering cholesterol through diet, medication, or both to keep your arteries clear.
Best Foods to Support Artery Health
Leafy Greens and Berries
Spinach, kale, and collard greens are rich in nitrates that improve blood vessel function. Add berries for antioxidants and anti-inflammatory benefits.
Omega-3 Rich Foods like Salmon
Omega-3 fatty acids reduce blood pressure and inflammation. Add salmon, sardines, or flaxseeds to your weekly meals.
Exercise and Movement to Keep Blood Flowing
Exercise Therapy are proven to improve symptoms. Even 30 minutes of walking daily helps retrain your arteries to deliver blood more efficiently.
Surgical and Minimally Invasive Procedures
In severe PAD, procedures like angioplasty (to open blocked arteries) or bypass surgery (to create a detour for blood flow) may be necessary. Northern Heart Hospital’s vascular team offers state-of-the-art techniques, including minimally invasive procedures that reduce recovery time.
How Northern Heart Hospital Can Help
At Northern Heart Hospital, our multidisciplinary approach ensures every patient gets a personalized care plan. From early screening and diagnostics to rehabilitation and surgery, we provide compassionate, expert care every step of the way.
Final Thoughts: Pay Attention to Your Legs Before It’s Too Late
Your legs are trying to tell you something. Do not brush off cramps, cold feet, or tired muscles. PAD is a serious condition, but with early detection and proper care, it is manageable and even reversible. Listen to your body and take the first step toward healthier arteries.
FAQs
1. Can PAD go away on its own?
No, PAD will not resolve on its own. However, lifestyle changes and treatment can stop it from getting worse and even reverse some symptoms.
2. Is PAD a sign of heart disease?
Yes, PAD and coronary artery disease often go hand in hand. If you have PAD, you are at higher risk for heart attack and stroke.
3. How is PAD different from deep vein thrombosis (DVT)?
PAD affects arteries and causes poor blood flow. DVT involves blood clots in veins, usually causing swelling and pain in one leg. Both are serious but different conditions.
4. Who should get screened for PAD?
Anyone over 50 with risk factors like smoking, diabetes, or high blood pressure should consider screening, especially if they have leg pain while walking.
5. Can children or teenagers get PAD?
It is rare, but not impossible, particularly in those with congenital conditions or genetic cholesterol disorders.
