How to Use a Home Blood Pressure Monitor Correctly
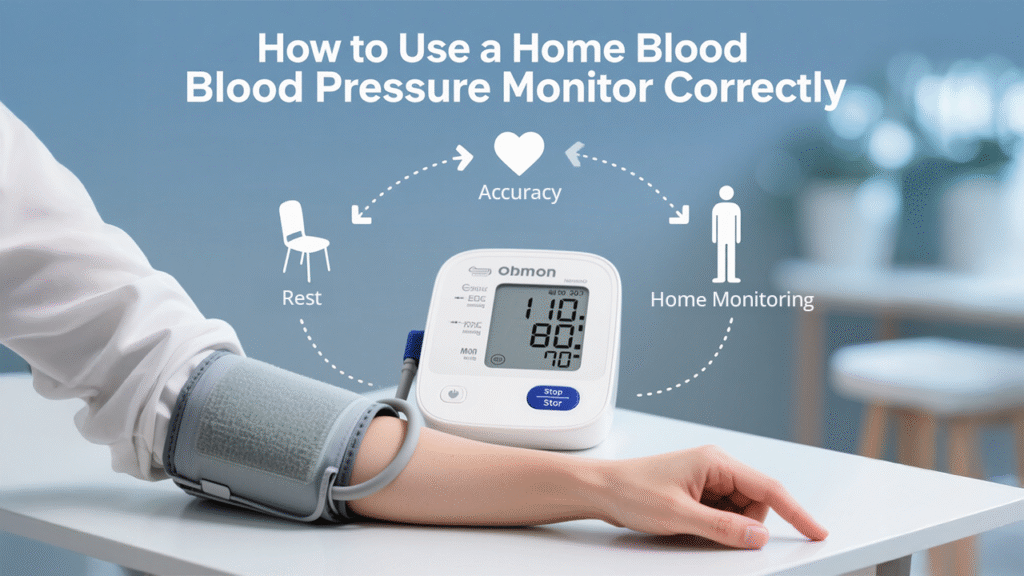
If you or a loved one has been told to monitor blood pressure at home, you are not alone. With hypertension being one of the top causes of heart disease and stroke, keeping tabs on your numbers is more than just good practice—it is essential. But here is the thing: the device is only as good as how you use it. Let us break it all down so you get accurate results every single time.
Why Monitoring Blood Pressure at Home Matters
Think of home blood pressure monitoring as your personal health radar. It helps detect trends, shows how your lifestyle changes are working, and alerts you and your doctor to potential problems early. Conditions like white coat hypertension (when readings are high at the doctor’s office but normal at home) or masked hypertension (the opposite) can go unnoticed without home monitoring.
At Northern Heart Hospital, specialists often encourage at-home monitoring to improve long-term outcomes and treatment accuracy.
Understanding Blood Pressure Readings
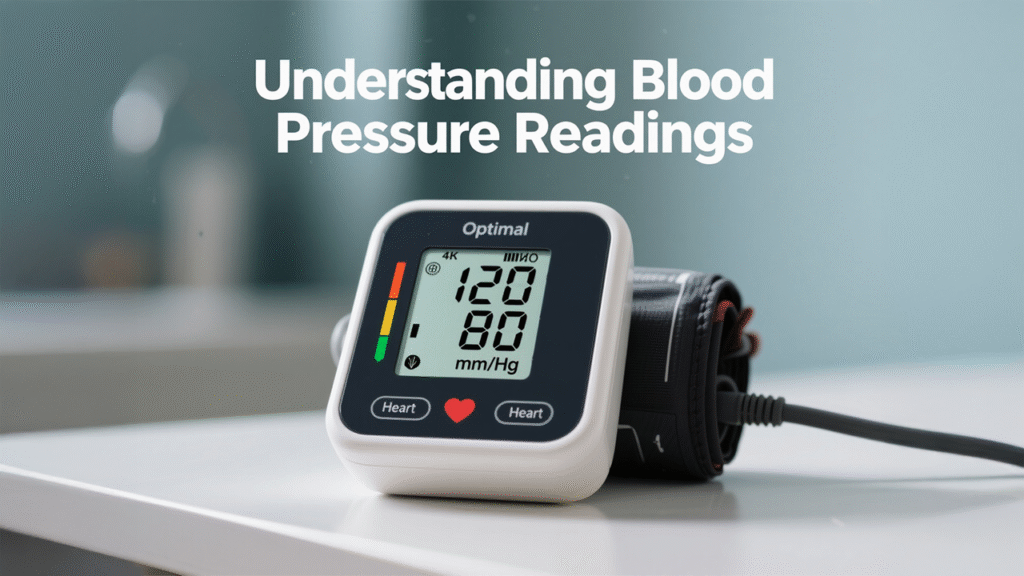
What Do the Numbers Mean?
Blood pressure readings include two numbers:
- Systolic (top number): Pressure when the heart beats.
- Diastolic (bottom number): Pressure when the heart rests.
A reading of 120/80 mmHg is considered optimal. The unit “mmHg” stands for millimeters of mercury—a nod to the first blood pressure devices.
What Is Considered Normal, High, or Low?
- Normal: Less than 120/80 mmHg
- Elevated: 120-129/<80 mmHg
- High (Stage 1): 130-139/80-89 mmHg
- High (Stage 2): 140+/90+ mmHg
- Hypertensive Crisis: 180+/120+ mmHg (Seek immediate medical help)
Consistently high readings mean your heart is working too hard. You can manage this, but only if you spot it early.
Types of Home Blood Pressure Monitors
Upper Arm Monitors vs. Wrist Monitors
Upper arm monitors are the gold standard. They are more reliable than wrist monitors, which can be affected by positioning and movement. At-home users should stick with validated upper arm models unless directed otherwise by a doctor.
Digital vs. Manual Monitors
Digital monitors are more user-friendly and suitable for most people. Manual devices (like those with a stethoscope and pump) require training. Unless you are a trained medical professional, go digital.
Choosing the Right Monitor for Your Needs

Before buying, consider:
- Cuff size: It must fit your upper arm properly.
- Validation: Look for devices certified by medical bodies (e.g. AAMI, BHS).
- Memory features: Some store previous readings automatically.
- Power source: Battery-operated or plug-in?
- Connectivity: Bluetooth options sync with health apps for tracking.
Talk to your healthcare provider or visit Northern Heart Hospital for guidance on choosing a trusted model.
Preparing to Take Your Blood Pressure
Time of Day and Environment
- Take readings at the same times each day—usually morning and evening.
- Sit in a quiet room with no distractions.
- Wait at least 30 minutes after exercise, meals, or caffeine.
What to Avoid Before a Reading
- No smoking, caffeine, or alcohol at least 30 minutes before.
- Empty your bladder.
- Sit quietly for five minutes before starting.
Your body needs to be in rest mode—not fight-or-flight mode—for accurate numbers.
Step-by-Step Guide to Using a Blood Pressure Monitor
· Step 1: Sit Comfortably and Relax
Place both feet flat on the floor. Sit upright with your back supported. Rest your arm on a flat surface (like a table) at heart level.
· Step 2: Position the Cuff Correctly
Wrap the cuff snugly around your upper arm (not over clothing). The cuff should sit one inch above your elbow. Most monitors have guides to help you position it correctly.
· Step 3: Start the Monitor and Stay Still
Press the start button and stay silent. Do not talk, move, or cross your legs. Movement can throw off your reading.
· Step 4: Record the Reading Accurately
Write down both numbers along with the time and date. Some devices save these for you. Keep a log or use a smartphone app if available. You can bring this record to your next Northern Heart Hospital appointment for a more complete health picture.
Common Mistakes to Avoid
- Improper cuff size: Too loose or tight? Your readings may be off.
- Wrong arm position: The cuff must be at heart level.
- Talking or moving during measurement: This raises your pressure.
- Measuring after stressful activity: Wait and cool off.
Even a great monitor can mislead you if used incorrectly.
How Often Should You Measure Blood Pressure?
If your doctor has not advised otherwise:
- Daily: Take two readings (morning and evening) for a week to establish a baseline.
- Long-term: 2–3 times per week is usually sufficient unless your condition requires closer monitoring.
Remember: consistency beats quantity. Follow a routine.
What to Do with Your Blood Pressure Readings
- Share them with your healthcare provider.
- Look for trends—not isolated spikes.
- If you see multiple readings above 140/90 mmHg, contact your doctor.
At Northern Heart Hospital, cardiologists use these records to fine-tune your medication and lifestyle plan.
When to Contact a Healthcare Professional
Call your doctor or go to the emergency room if:
- You consistently get readings above 180/120 mmHg.
- You feel dizzy, confused, short of breath, or have chest pain.
- Your blood pressure fluctuates wildly without reason.
It is not just about the numbers, but how you feel too.
How Northern Heart Hospital Supports Hypertension Management
From diagnosis to ongoing support, Northern Heart Hospital provides expert care for patients with high blood pressure. Our team offers comprehensive evaluations, personalized plans, medication management, and lifestyle coaching to help you take control of your cardiovascular health.
Final Thoughts: Take Control of Your Numbers Before They Control You
Using a home blood pressure monitor might seem simple, but doing it right makes all the difference. It is one of the most powerful tools you have for protecting your heart—right up there with eating well and staying active. Your numbers tell a story. Make sure you are reading it correctly.
FAQs
1. Should I measure blood pressure on the left or right arm?
Most doctors recommend the left arm since it is closer to the heart. However, use the arm with the higher reading if instructed otherwise by your doctor.
2. How long should I wait between readings?
Wait one to two minutes between readings if taking more than one. Always take the average of two readings for better accuracy.
3. Can stress or anxiety affect my readings?
Absolutely. Emotional stress can raise your pressure temporarily. If you are feeling anxious, take a few deep breaths and try again after a short rest.
4. Is it okay to measure blood pressure after exercise?
No, it is best to wait at least 30 minutes after physical activity. Post-exercise readings are often inaccurate due to elevated heart rate and pressure.
5. How do I know if my monitor is accurate?
Get it checked at your doctor’s office. Bring it along to your next appointment at Northern Heart Hospital and compare it to their calibrated machines.
